In the coming days/weeks, you’re going to hear a lot about how Ukraine should accept the terms of surrender (as that’s what they are) offered by Russia—how they’d be “stupid” not to, how Zelenskyy should “do the right thing for his people” and prioritize saving lives, how peace should be the priority and we can’t always get what we want.
Make no mistake: even if Russia intends to uphold these terms once Zelenskyy accepts them, this is a terrible deal for Ukraine and a terrible deal for the world.
First of all, there’s no guarantee that Russia will respect a cease fire or peace treaty. Obviously that’s always the case with war, but it’s especially the case when they’ve already violated multiple cease fire agreements by firing on and murdering evacuating civilians, including children. So there’s your peace treaty.
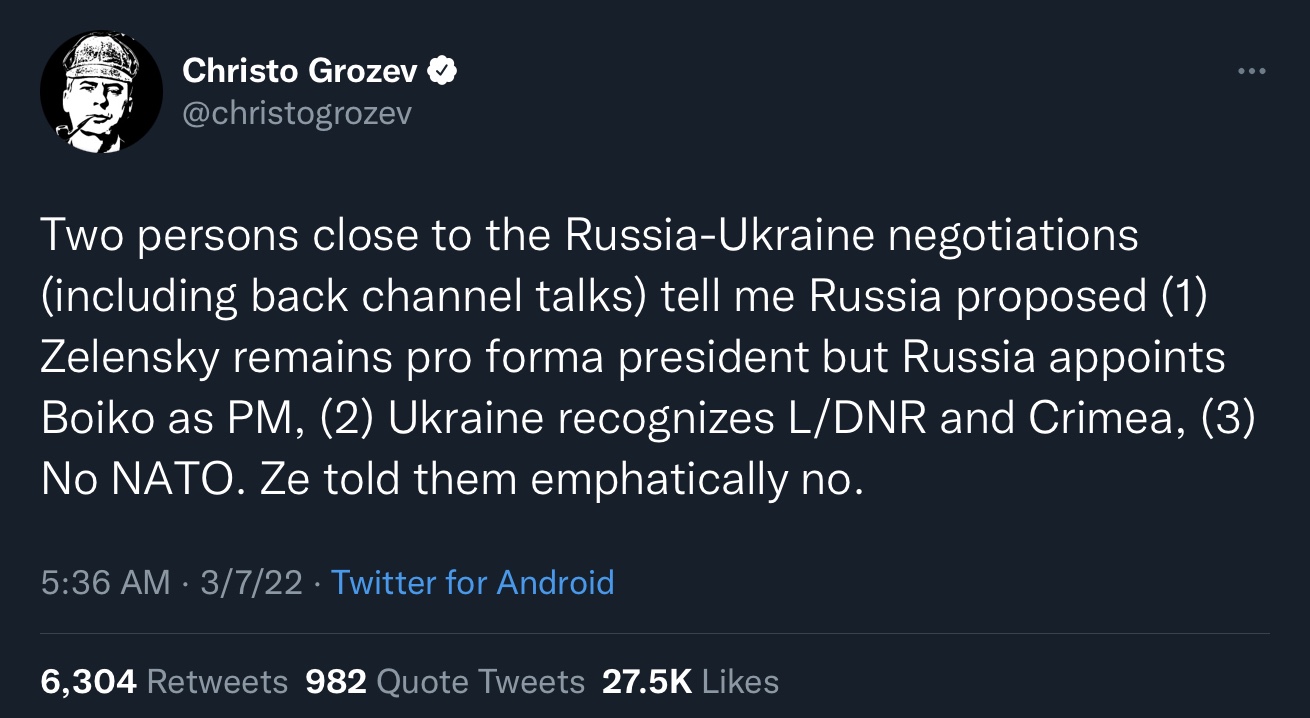
Second, the terms that Russia has presented include virtually all of Putin’s actual goals for this illegal invasion (obviously “de-Nazification” and “de-militarization” were just lies à la “weapons of mass destruction,” a rhetorical tactic that really ought to be familiar to any self-respecting American leftist). Ukraine would forfeit its claim on the territories Russia has already illegally annexed/recognized, it would be forced to change its constitution (!!!) to commit to never joining any “pacts” (EU, NATO, anything else that forms in the future), and it would retain Zelenskyy as a figurehead while installing a pro-Russian actual government leadership.
This is—and I cannot stress this enough—not a “compromise” or a “peace treaty.” It’s terms of surrender. And the lesson learned here is that Russia can continue invading and terrorizing sovereign states without any actual consequences—remember, Putin doesn’t personally care about Western sanctions. He doesn’t care if his people are plunged into poverty as long as he and his cronies aren’t, and they won’t be. He’s furious about the sanctions because he finds them personally offensive and because they confirm his victim complex, not because he’s legitimately worried for his people like Zelenskyy is.
Third, and perhaps most importantly, Putin has made it extremely clear that he seeks to rebuild a Russian empire. He will not stop with Crimea, Luhansk, and Donetsk. (And make no mistake—Luhansk and Donetsk are not independent sovereign states like Ukraine; they’re simply Russian satellites.) He will not stop with forced regime change in Belorus, Georgia, Syria, and Ukraine. (And even if he did—isn’t that awful enough?) He is not “concerned about Russia’s security” or “worried about NATO’s encroachment” or whatever his extensive social media operation has you believing. He’s not concerned or worried about anything. He’s a dictator expanding his empire. He is exactly what you all feared Trump was.
I believe that this “offer” from Russia to Ukraine serves two purposes, and neither of them is to establish a lasting peace and autonomy for each country. One is to give Putin a potential way to back out of a war that has already gone much worse than he expected and cost him significantly in terms of personnel and equipment. (Not the sanctions—like I said, I don’t think he personally cares about the sanctions and in fact sees them as a political tool to use to his advantage.)
The second and more important goal is to create a way for the international community to blame Ukraine for the continued war. “If you’d just accept the terms, you could save your people and prevent nuclear war.” It’s absolutely classic DARVO tactics that, again, any progressive activist should be familiar with. “Sure, it’s not your fault he attacked you, but you shouldn’t have reported itmade a big deal of itgotten him “cancelled”made it publicetc.”
It’s not Ukraine’s responsibility to “prevent nuclear war.” Ukraine gave up its nuclear weapons in exchange for protection—protection that it has not received, although Western aid and military assistance has undoubtedly been helpful. Placing responsibility on Ukraine to accept unjust terms and illegal annexation of its land in order to “prevent nuclear war” only lends credence to the claim that only nuclear weapons can keep a country truly safe—after all, it would mean that Putin’s nuclear threats have allowed him to invade his neighbors, terrorize their citizens, destroy their resources, replace their democratically elected leaders with his own puppets, and steal their land—without even having to make any concessions himself.
So here’s my plea to my American progressive/leftist siblings. Please question what you think you know about Putin, Russia, and Ukraine. There are certainly far-right and neo-Nazi political forces in Ukraine as there are in any country, but Zelenskyy is a progressive, democratically elected JEWISH president. NATO and the EU have their (serious) issues, but they have not pressured or forced any former Soviet states to join—in fact, prior to this war, it seemed unlikely that Ukraine would be admitted. Ukraine WANTED to join to protect itself from Russia, which had already illegally annexed its land, empowered far-right groups within its borders, and forced regime changes in surrounding countries.
Putin is not an anti-imperialist revolutionary; he denounces American imperialism because it’s convenient for him politically and it keeps the American left from putting pressure on our government to divest from Russia. Sure, maybe the Democrats oversold Russian election hacking as an explanation for Trump’s win (although the more I learn about the extent of Russia’s disinfo campaign, the more I question this common leftist talking point), but that doesn’t mean that Putin isn’t bent on conquering Eastern Europe and subduing Western powers by any means necessary. This goes far beyond American electoral politics, and the answers here do not conform to American party lines. Do not fall into the trap of dismissing politicians’ statements about Putin and Russia just because you disagree with the rest of their stances.
Putin is a dictator. Sometimes it really is that simple. A former KGB agent, he came to power by staging the modern Russian version of the Reichstag fire (look up “Russian apartment bombings”), using that as an excuse to start a war and win it, and he has maintained his power through strong-arming and terror. The State Duma is entirely symbolic at this point; anyone who goes against Putin knows that they are likely not only to die, but to die horribly, just like Alexei Navalny almost did not long ago (look up “Novichok” and prepare yourself for some body horror).
I could go on. I won’t right now. But in truth, I deeply regret the fact that I haven’t done more over the past 8 or so years to disrupt the blatant Putinist propaganda I hear from a lot of my fellow progressives. I had other priorities and I didn’t give it the attention I should’ve. To be clear: nothing America or American progressives could’ve done would’ve stopped this war, only delayed it or hastened it. The war was inevitable because Putin wants to conquer Ukraine, and beyond.
So I’ll just say—please, please listen to people who fled Russia/the Soviet Union, and to experts who study Russia. The most likely threat here isn’t a nuclear WWIII; this isn’t about you. The thing people like me fear most is simply that Putin will continue subjugating, terrorizing, and ultimately conquering innocent citizens of sovereign states, and that the West will eventually just accept this as the price of nuclear deterrence.
I’m not a political scientist; I don’t know how to stop this war. All I know is that Ukrainian surrender isn’t it. Listen to Ukrainians, anti-Putin Russians, and other experts, form your own opinion, and most importantly, keep your wits about you. Not everyone in this world is a good faith negotiating partner. Some people are, unfortunately, just evil. Hitler was, Stalin was, Putin is.